Understanding Hip Bursitis
Causes, Anatomy, and Effective Treatment
by Krisitn Cameron09 Nov 2025
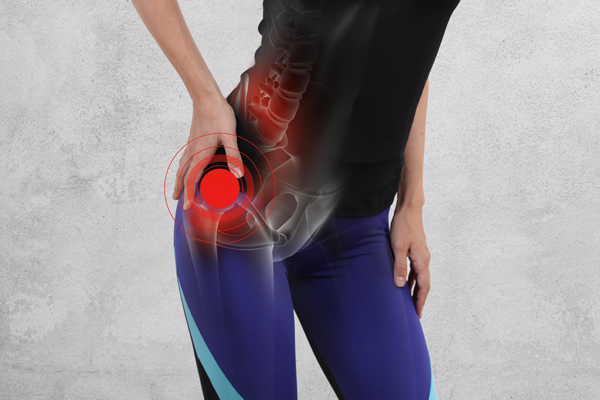
Hip bursitis is a common source of outer hip pain. It affects people of all ages, from active individuals and runners to those who spend long hours sitting or standing. While symptoms can appear suddenly, hip bursitis often develops gradually due to muscle imbalances, movement dysfunction, or overuse.
Early assessment and Physiotherapy treatment for hip pain can make a significant difference, helping to resolve pain quickly and prevent it from becoming a long-term issue.
Anatomy of the Hip and the Bursa
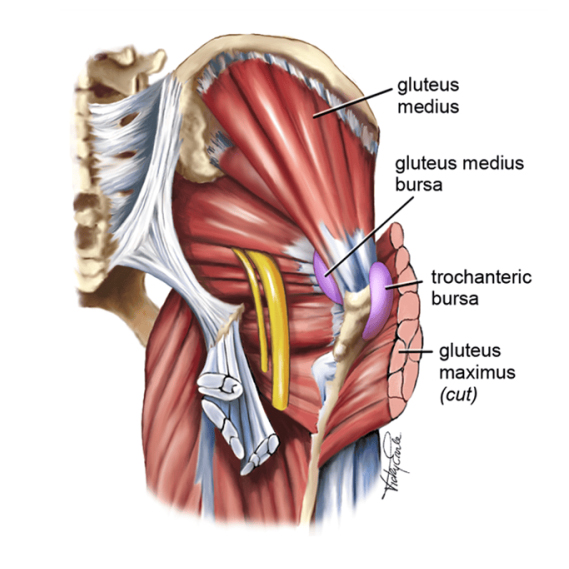
The bursa is a small, fluid-filled sac that cushions movement between bones and soft tissue. Around the hip, several bursae provide this protection, but the most commonly affected is the greater trochanteric bursa, located over the bony prominence on the outer hip (the greater trochanter).
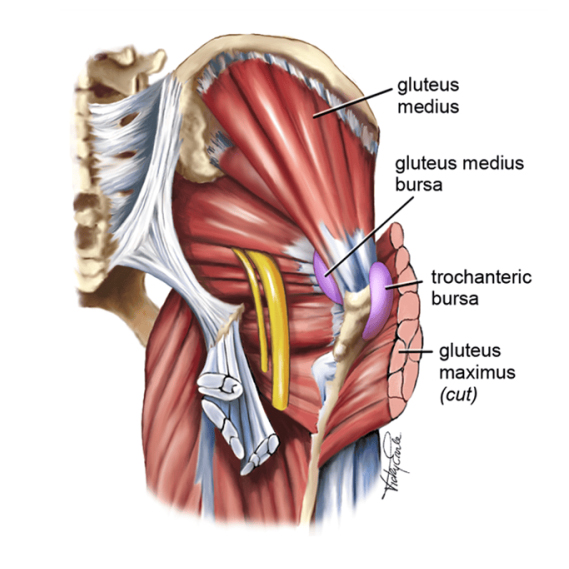
Other nearby structures that often contribute to hip pain include:
Gluteus medius tendon – a key stabiliser of the pelvis during walking and single-leg activities.
Gluteus minimus tendon – assists in hip abduction and control.
Iliotibial band (ITB) – a fibrous band running down the outer thigh that can compress the bursa if tight or overactive.
When gluteal tendons are weak or the ITB is tight, friction and compression can irritate the bursa, leading to inflammation and pain.
Common Causes of Hip Bursitis
Hip bursitis usually develops from repetitive stress, poor biomechanics, or muscle imbalance. A common example is performing exercises like squats, lunges, or step-ups with poor hip control, which increases pressure on the bursa.

The knee rolling inward (valgus collapse) during movement.
The opposite hip dropping, showing weak pelvic stability
Strong gluteus maximus and quadriceps, but an underactive gluteus medius.
These issues increase friction over the greater trochanter and lead to irritation of the surrounding tendons and bursa. Over time, even simple activities like climbing stairs or walking uphill can become painful.
Repetitive activities such as running or cycling.
Weakness in the hip stabilisers, particularly the gluteus medius
Sudden increases in training intensity or load.
Poor posture or altered walking mechanics
Direct trauma or impact to the hip.
Age-related tendon changes.
Recognising the Symptoms
People with hip bursitis often report:
Pain or tenderness on the outside of the hip, sometimes radiating down the thigh.
Discomfort when lying on the affected side.
Pain when walking, climbing stairs, or standing on one leg.
Tenderness directly over the greater trochanter.
Pain that worsens after exercise or prolonged sitting.
Hip Bursitis Treatment and Recovery
Modify or avoid aggravating activities, such as deep squats or side-lying positions
Apply ice to the outer hip for 15-20 minutes to reduce pain.
In some cases, your GP or Physiotherapist may suggest a corticosteroid injection for short-term relief.

Stand side-on to a wall with a small ball or towel between your inner knee and the wall.
Press gently into the ball while keeping your pelvis level.
Slightly bend the supporting knee into a semi-squat.
Hold for 10-30 seconds, repeat 3 times per side.
Keep your knees level, don’t let the opposite hip drop
Avoid your knee rolling inward.
Focus on control and slow, steady activation.
This simple but effective exercise helps switch the gluteus medius back on, improving hip control and reducing load on the bursa.

Stand on a step or box.
Slowly lower the opposite foot toward the floor while keeping your knee aligned over your foot.
Keep your hips level and your movement controlled.
Return to standing and repeat.
This exercise strengthens the gluteal muscles and improves hip stability during single-leg movement.
Step-ups or single-leg squats (with correct alignment).
Glute bridges, progressing to single leg.
Crab walk and other banded resistance exercises.
Functional exercises tailored to your activity or sport.
Quality movement always comes before resistance. Building strength on top of poor mechanics can easily cause symptoms to return.
Prevention Tips for Hip Bursitis
To reduce your risk of recurrence:
Include gluteal and core strengthening in your regular routine.
Avoid lying on the affected side for extended periods.
Regularly stretch your ITB, hip flexors, and quads.
Monitor your form during exercises. A physiotherapist can help with this.
Gradually increase your training load and avoid sudden spikes in activity.
When to Seek Professional Help

If you begin to experience outer hip pain or tenderness, it’s best to see a physiotherapist early, not only if the pain becomes severe or persistent.
Early assessment allows your physiotherapist to identify underlying causes such as gluteal weakness, hip control issues, or biomechanical imbalance before the condition worsens. Addressing these factors early helps reduce recovery time, prevent inflammation, and lower the risk of chronic symptoms.
A Physiotherapist can perform a detailed movement and gait assessment, prescribe tailored exercises for hip bursitis, and guide you on proper technique to offload the irritated tissues. Early physiotherapy intervention leads to faster recovery, improved movement, and long-term prevention.
Key Takeaways
Hip bursitis is often the result of poor hip stability and muscle imbalance rather than a single injury.
By improving gluteal strength, correcting movement patterns, and addressing pain early through physiotherapy, most people make a full recovery and return to their normal activities without discomfort.
Still in pain? We can help.
If your hip pain or bursitis isn’t easing with these gentle exercises, see our experienced Physiotherapists at Physio Fitness Bondi Junction.
👉 Book your consultation today or call us on (02) 9389 9100 to start your recovery.

Early assessment and Physiotherapy treatment for hip pain can make a significant difference, helping to resolve pain quickly and prevent it from becoming a long-term issue.
Anatomy of the Hip and the Bursa
The bursa is a small, fluid-filled sac that cushions movement between bones and soft tissue. Around the hip, several bursae provide this protection, but the most commonly affected is the greater trochanteric bursa, located over the bony prominence on the outer hip (the greater trochanter).
Common Causes of Hip Bursitis
Hip bursitis usually develops from repetitive stress, poor biomechanics, or muscle imbalance. A common example is performing exercises like squats, lunges, or step-ups with poor hip control, which increases pressure on the bursa.

This may look like:
Other contributing factors include:
Recognising the Symptoms
People with hip bursitis often report:
Hip Bursitis Treatment and Recovery
1. Reduce Inflammation
2. Restore Hip Control and Gluteal Activation
Exercise 1: One leg ball squat (Isometric)

Key tips:
Exercise 2: Controlled Step-Down
After regaining basic control, progress to eccentric (lowering) strength work.
3. Progressive Strengthening
Prevention Tips for Hip Bursitis
To reduce your risk of recurrence:
When to Seek Professional Help

Early assessment allows your physiotherapist to identify underlying causes such as gluteal weakness, hip control issues, or biomechanical imbalance before the condition worsens. Addressing these factors early helps reduce recovery time, prevent inflammation, and lower the risk of chronic symptoms.
A Physiotherapist can perform a detailed movement and gait assessment, prescribe tailored exercises for hip bursitis, and guide you on proper technique to offload the irritated tissues. Early physiotherapy intervention leads to faster recovery, improved movement, and long-term prevention.
Key Takeaways
Hip bursitis is often the result of poor hip stability and muscle imbalance rather than a single injury.
By improving gluteal strength, correcting movement patterns, and addressing pain early through physiotherapy, most people make a full recovery and return to their normal activities without discomfort.
Still in pain? We can help.
If your hip pain or bursitis isn’t easing with these gentle exercises, see our experienced Physiotherapists at Physio Fitness Bondi Junction.
👉 Book your consultation today or call us on (02) 9389 9100 to start your recovery.

B.Phty (Cred), APAM
Senior Physiotherapist
Senior Physiotherapist



